Pulmonary Function Test for Asthma: Understanding the Importance, Procedure, and Benefits
Discover the significance of a pulmonary function test (PFT) for asthma, its role in diagnosis, procedure, and how it helps in managing asthma effectively.

Introduction
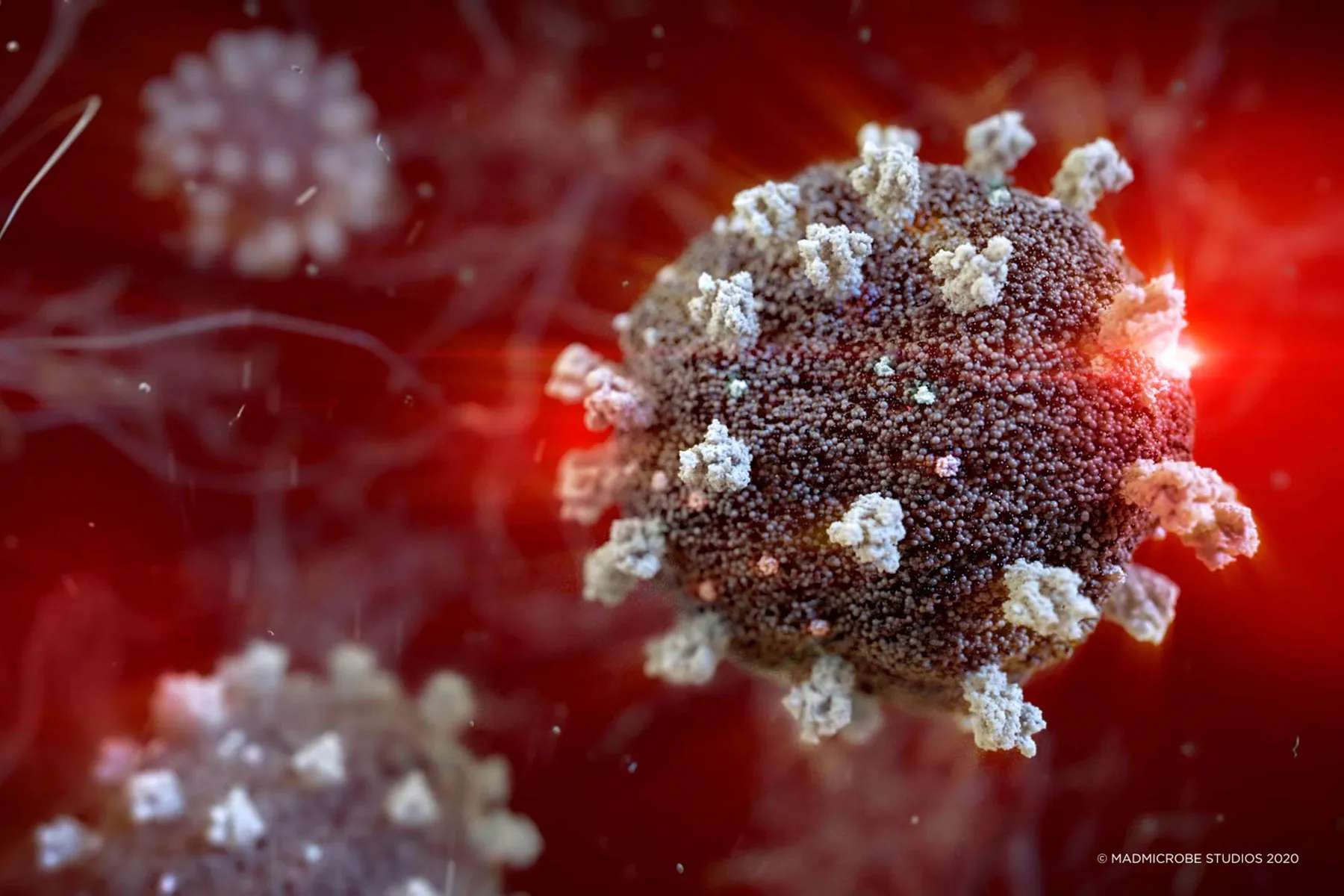
Asthma, a chronic respiratory condition that causes the airways to narrow and swell, affecting millions worldwide, requires careful management and monitoring. One of the most effective ways to assess asthma and track lung function is through a pulmonary function test (PFT). A pulmonary function test for asthma provides essential insights into lung health, helping healthcare providers design personalized treatment plans.
In this article, we'll explore the significance of pulmonary function tests for asthma, the procedure involved, and the benefits they offer for individuals living with this condition.
What is a Pulmonary Function Test?
A pulmonary function test (PFT) is a non-invasive procedure used to assess the functioning of the lungs. It measures the volume of air a person can inhale and exhale, how quickly air can be expelled from the lungs, and the efficiency of gas exchange within the lungs. For people with asthma, PFTs are crucial for evaluating the extent of lung impairment, monitoring disease progression, and adjusting treatment plans accordingly.
Types of Pulmonary Function Tests Used for Asthma
There are several types of pulmonary function tests, each designed to measure different aspects of lung function. The two primary tests used in asthma management are:
-
Spirometry
- Spirometry is the most common and widely used pulmonary function test for asthma. It measures the amount and speed of air a person can breathe out. The key measurements include:
- Forced Vital Capacity (FVC): The total volume of air exhaled after taking a deep breath.
- Forced Expiratory Volume in 1 second (FEV1): The amount of air exhaled during the first second of the forced exhalation.
- FEV1/FVC ratio: This ratio helps to assess the degree of airway obstruction.
- Spirometry is the most common and widely used pulmonary function test for asthma. It measures the amount and speed of air a person can breathe out. The key measurements include:
-
Peak Expiratory Flow (PEF) Test
- A Peak Flow Meter is used to measure the maximum speed at which a person can force air out of their lungs. Monitoring peak flow can help asthma patients detect early signs of an asthma attack.
-
Lung Volume Measurement
- This test measures the total amount of air the lungs can hold, which is particularly useful for diagnosing certain types of lung diseases.
-
Diffusing Capacity for Carbon Monoxide (DLCO) Test
- The DLCO test measures how well gases such as oxygen move from the lungs into the bloodstream. It’s often used in patients with chronic respiratory diseases to assess lung efficiency.
Why is a Pulmonary Function Test Important for Asthma?
A pulmonary function test is a cornerstone in asthma management because it provides valuable data that can influence the treatment approach. Here are several reasons why PFTs are essential for asthma patients:
-
Early Diagnosis of Asthma
- Early diagnosis is critical for effective asthma management. A pulmonary function test can identify abnormal lung function in the early stages of asthma, even before symptoms become severe. Detecting asthma early can prevent long-term lung damage.
-
Monitoring Asthma Progression
- Asthma symptoms can fluctuate over time, and lung function may deteriorate during flare-ups. PFTs help track changes in lung function, allowing healthcare providers to adjust treatment plans based on current health status.
-
Assessing the Effectiveness of Treatment
- Pulmonary function tests help determine whether asthma medications, such as inhalers or oral corticosteroids, are working effectively. Improvement in lung function after using a bronchodilator during spirometry, for example, can indicate that the medication is helping open up the airways.
-
Determining the Severity of Asthma
- By assessing FEV1 and FVC measurements, PFTs can classify asthma as mild, moderate, or severe, providing an objective basis for treatment decisions.
-
Preventing Asthma Exacerbations
- Regular monitoring of pulmonary function allows healthcare providers to spot early signs of an impending asthma exacerbation. Early intervention can prevent severe attacks and reduce the risk of hospitalization.
The Procedure: What to Expect During a Pulmonary Function Test
Undergoing a pulmonary function test is generally a straightforward and quick process. Here's what you can expect during the test:
-
Preparation
- Before the test, your healthcare provider may advise you to avoid certain medications, such as bronchodilators or corticosteroids, for several hours. It’s also important to refrain from smoking or strenuous exercise before the test to ensure accurate results.
-
Spirometry
- During a spirometry test, you will be asked to take a deep breath and then blow out as hard and fast as you can into a mouthpiece connected to a spirometer. The test may be repeated several times to ensure accuracy. In some cases, a bronchodilator may be administered to assess its effect on lung function.
-
Peak Flow Measurement
- A peak flow meter is a small handheld device that you will be asked to blow into. The peak flow measurement will be recorded, and the results will be compared to your previous readings.
-
Lung Volume Measurement
- This test requires you to breathe in a gas or air through a mouthpiece, and then measurements of lung volumes are taken.
-
Post-Test Evaluation
- After the test, your healthcare provider will analyze the results, compare them to normal values, and determine how your lung function measures up. They may also recommend further testing if needed.
Benefits of Pulmonary Function Testing for Asthma
Pulmonary function tests offer numerous benefits for individuals living with asthma:
-
Personalized Asthma Management
- By understanding how asthma affects lung function, healthcare providers can tailor treatment plans to the individual, choosing medications and therapies that will be most effective.
-
Early Detection of Asthma Complications
- Regular monitoring with pulmonary function tests can identify complications or coexisting conditions, such as chronic obstructive pulmonary disease (COPD), which can worsen asthma.
-
Improved Quality of Life
- By optimizing asthma management, PFTs help patients maintain better control over their symptoms, leading to improved day-to-day functioning and quality of life.
-
Prevention of Long-Term Lung Damage
- Long-term uncontrolled asthma can lead to permanent lung damage. Regular testing ensures that any changes in lung function are identified early, helping prevent permanent damage.
FAQs About Pulmonary Function Tests for Asthma
1. How often should I undergo a pulmonary function test for asthma?
It’s generally recommended to have a pulmonary function test annually or more frequently if your asthma symptoms change, worsen, or if your healthcare provider suggests it.
2. Can I eat before a pulmonary function test?
It’s typically fine to eat before the test, but avoid heavy meals that may affect your breathing. Be sure to follow any specific instructions given by your healthcare provider.
3. Are there any risks associated with pulmonary function testing?
Pulmonary function tests are generally safe. Some individuals may feel lightheaded or tired after the test, but serious complications are rare.
4. Can a pulmonary function test diagnose asthma on its own?
While a pulmonary function test is a valuable diagnostic tool, it is typically used in conjunction with your medical history and physical examination to confirm an asthma diagnosis.
5. What should I do if my test results indicate worsening lung function?
If your test results show decreased lung function, consult your healthcare provider immediately. They will help adjust your treatment plan to better manage your asthma.
Conclusion
A pulmonary function test for asthma is an essential tool in diagnosing, managing, and monitoring asthma. Through tests like spirometry, peak flow measurement, and lung volume testing, healthcare providers can gain valuable insights into lung health and adjust treatments accordingly. With the ability to track asthma progression and assess medication effectiveness, pulmonary function tests help prevent exacerbations, reduce symptoms, and improve the overall quality of life for asthma patients.
If you're living with asthma, consider scheduling regular pulmonary function tests to ensure optimal management of your condition and enjoy a healthier, more active life.
What's Your Reaction?